Our Services
Complete Cardiovascular Care in Statesboro, Metter, Swainsboro and Reidsville, GA.
At Statesboro Cardiology Vascular and Vein Specialists, we take a patient-focused, collaborative approach to your heart care. Our specialists use their years of combined knowledge and expertise to get you the best care cardiology has to offer, so you can have the peace of mind you deserve. For us, that not only means giving you access to industry-leading procedures and equipment, but it also means that we take the time to build a caring relationship with you and your family. When it comes to the heart, excellent care is essential.

General Cardiology
If you have been referred by your primary care physician, you have a family history of heart disease, you are a smoker, you have high cholesterol, blood pressure, or diabetes, you have a history of preeclampsia, or a congenital heart defect, you need a cardiologist. When your heart health is at stake, the best choice is to let your cardiologist do the listening and help you keep the conversation strong and clear.

Interventional Cardiology
When the plumbing of your heart gets clogged, the interventional cardiologists at Statesboro Cardiology should be your first call. For coronary artery disease, heart valve disease, peripheral vascular disease, and congenital heart defects, our interventional cardiologists have very specialized training that enables them to utilize catheters to clear the path for your blood to flow the way it should.

Electrophysiology
When it comes to your heart, “skipping a beat” isn’t really a good thing. Fainting, chest pain, fluttering in the chest, and dizziness could be indications of Arrhythmia, or an irregular heart beat.
Our Electrophysiology service can help you get back on beat, and feeling like yourself again.

Vein Ablation
Large veins visible just under the surface of your skin, mild swelling of your ankles and feet, throbbing, cramping or “heavy” legs, or clusters of red veins on your upper body or face or legs may be signs of weakened veins caused by venous insufficiency. Vein ablation is used to treat varicose veins and spider veins and prevent the drastic complications that arise as a result. This treatment can have your legs looking and feeling younger in no time.
Our Cardiology Services include
Arterial and Venous Ultrasounds
Arterial and Venous Ultrasounds
Catheter Ablation
Your doctor may recommend ablation if:
The medicines you take don’t control your arrhythmia.
You can’t tolerate the medicine your doctor has prescribed for your arrhythmia.
You have certain types of arrhythmia. (Your doctor can tell you whether catheter ablation can help treat your arrhythmia.)
You have faulty electrical activity in your heart that raises your risk of ventricular fibrillation (v-fib) and sudden cardiac arrest (SCA). V-fib is a life-threatening arrhythmia. SCA is a condition in which your heart suddenly stops beating.
Outlook
Catheter ablation alone doesn’t always restore a normal heart rate and rhythm. You may need other treatments as well. Also, some people who have the procedure may need to have it done again. This can happen if the first procedure doesn’t fully correct the problem.
Catheter ablation is also known as:
Ablation
Cardiac ablation
Cardiac catheter ablation
Radiofrequency ablation
Catheter cryoablation
Clinic/Consultation
Located at our 5 Grady Johnson Road office location and staffed daily by one of our cardiologists, we offer our patients appointments for urgent cardiac or peripheral vascular concerns, pre-operative clearance and noninvasive testing.
Coronary and Peripheral Angiography
Coronary angioplasty (AN-jee-oh-plas-tee) is a procedure used to open blocked or narrowed coronary (heart) arteries. The procedure improves blood flow to the heart muscle.
Over time, a fatty substance called plaque (plak) can build up in your arteries, causing them to harden and narrow. This condition is called atherosclerosis (ath-er-o-skler-O-sis).
Atherosclerosis can affect any artery in the body. When atherosclerosis affects the coronary arteries, the condition is called coronary heart disease (CHD) or coronary artery disease.
Angioplasty can restore blood flow to the heart if the coronary arteries have become narrowed or blocked because of CHD.
Angioplasty is a common medical procedure. It may be used to:
Improve symptoms of CHD, such as angina (an-JI-nuh or AN-juh-nuh) and shortness of breath. (Angina is chest pain or discomfort.)
Reduce damage to the heart muscle caused by a heart attack. A heart attack occurs if blood flow through a coronary artery is completely blocked. The blockage usually is due to a blood clot that forms on the surface of plaque. During angioplasty, a small balloon is expanded inside the coronary artery to relieve the blockage.
Reduce the risk of death in some patients.
Angioplasty is done on more than 1 million people a year in the United States. Serious complications don’t occur often. However, they can happen no matter how careful your doctor is or how well he or she does the procedure.
Research on angioplasty is ongoing to make it safer and more effective, to prevent treated arteries from narrowing again, and to make the procedure an option for more people.
What Is a Stent?
A stent is a small mesh tube that’s used to treat narrow or weak arteries. Arteries are blood vessels that carry blood away from your heart to other parts of your body.
A stent is placed in an artery as part of a procedure called percutaneous (per-ku-TA-ne-us) coronary intervention (PCI), sometimes referred to as coronary angioplasty (AN-jee-oh-plas-tee). PCI restores blood flow through narrow or blocked arteries. A stent helps support the inner wall of the artery in the months or years after PCI. Doctors also may place stents in weak arteries to improve blood flow and help prevent the arteries from bursting. Stents usually are made of metal mesh, but sometimes they’re made of fabric. Fabric stents, also called stent grafts, are used in larger arteries. Some stents are coated with medicine that is slowly and continuously released into the artery. These stents are called drug-eluting stents. The medicine helps prevent the artery from becoming blocked again.
For the Coronary Arteries
Doctors may use stents to treat coronary heart disease (CHD). CHD is a disease in which a waxy substance called plaque (plak) builds up inside the coronary arteries. These arteries supply your heart muscle with oxygen-rich blood. When plaque builds up in the arteries, the condition is called atherosclerosis (ath-er-o-skler-O-sis).
Plaque narrows the coronary arteries, reducing the flow of oxygen-rich blood to your heart. This can lead to chest pain or discomfort called angina (an-JI-nuh or AN-juh-nuh). The buildup of plaque also makes it more likely that blood clots will form in your coronary arteries. If blood clots block a coronary artery, a heart attack will occur. Doctors may use percutaneous coronary intervention (PCI) (sometimes referred to as coronary angioplasty) and stents to treat CHD. During PCI, a thin, flexible tube with a balloon or other device on the end is threaded through a blood vessel to the narrow or blocked coronary artery. Once in place, the balloon is inflated to compress the plaque against the wall of the artery. This restores blood flow through the artery, which reduces angina and other CHD symptoms. Unless an artery is too small, a stent usually is placed in the treated portion of the artery during PCI. The stent supports the artery’s inner wall. It also reduces the chance that the artery will become narrow or blocked again. A stent also can support an artery that was torn or injured during PCI. Even with a stent, there’s about a 10–20 percent chance that an artery will become narrow or blocked again in the first year after PCI. When a stent isn’t used, the risk can be as much as 10 times as high. Research has shown that as time goes by, people who have coronary artery stents are in less danger of risks from the surgery but more prone to the risks of chronic diseases, such as type 2 diabetes and renal failure.
For Other Arteries
Plaque also can narrow other arteries, such as those in the kidneys and limbs. Narrow kidney arteries can affect kidney function and lead to severe high blood pressure. Narrow arteries in the limbs, a condition called peripheral arterial disease (P.A.D.), can cause pain and cramping in the affected arm or leg. Severe narrowing can completely cut off blood flow to a limb, which could require surgery. To relieve these problems, doctors may do PCI on a narrow kidney, arm, or leg artery. They often will place a stent in the affected artery during the procedure. The stent helps support the artery and keep it open.
Source: National Heart, Lung, and Blood Institute; National Institutes of Health; U.S. Department of Health and Human Services.
Coronary and Peripheral Stent Placement
Echocardiography
Echo also can pinpoint areas of heart muscle that aren’t contracting well because of poor blood flow or injury from a previous heart attack. A type of echo called Doppler ultrasound shows how well blood flows through your heart’s chambers and valves.
Echo can detect possible blood clots inside the heart, fluid buildup in the pericardium (the sac around the heart), and problems with the aorta. The aorta is the main artery that carries oxygen-rich blood from your heart to your body.
Source: National Heart, Lung, and Blood Institute; National Institutes of Health; U.S. Department of Health and Human Services.
Electrophysiological Studies
An arrhythmia (ah-RITH-me-ah) is a problem with the rate or rhythm of the heartbeat. During an arrhythmia, the heart can beat too fast, too slow, or with an irregular rhythm. A heartbeat that is too fast is called tachycardia (TAK-ih-KAR-de-ah). A heartbeat that is too slow is called bradycardia (bray-de-KAR-de-ah). Most arrhythmias are harmless, but some can be serious or even life threatening. During an arrhythmia, the heart may not be able to pump enough blood to the body. Lack of blood flow can damage the brain, heart, and other organs.
What is an Electrophysiology study (EPS)?
This test is used to assess serious arrhythmias. During an EPS, a thin, flexible wire is passed through a vein in your groin (upper thigh) or arm to your heart. The wire records your heart’s electrical signals.
Your doctor can use the wire to electrically stimulate your heart and trigger an arrhythmia. This allows your doctor to see whether an anti-arrhythmia medicine can stop the problem.
Source: National Heart, Lung, and Blood Institute; National Institutes of Health; U.S. Department of Health and Human Services.
Exercise Stress Test
Source: National Heart, Lung, and Blood Institute; National Institutes of Health; U.S. Department of Health and Human Services.
Heart Failure Clinic
In the Heart Failure Clinic at Statesboro Cardiology, our trained providers are committed to stratifying the care of patients who are at risk for heart failure and for those who have been diagnosed with heart failure.
The goal of our Heart Failure Clinic is to optimize patient’s medical therapy, manage patient’s heart failure conditions, and provide education specifically to detect any changes in cardiovascular status. Ultimately our goal is to help our patients who have this condition live a longer and more active life.
What Is Heart Failure?
Heart failure is a condition in which the heart can’t pump enough blood to meet the body’s needs. In some cases, the heart can’t fill with enough blood. In other cases, the heart can’t pump blood to the rest of the body with enough force. Some people have both problems. The term “heart failure” doesn’t mean that your heart has stopped or is about to stop working. However, heart failure is a serious condition that requires medical care.
Overview
Heart failure develops over time as the heart’s pumping action grows weaker. The condition can affect the right side of the heart only, or it can affect both sides of the heart. Most cases involve both sides of the heart.
Right-side heart failure occurs if the heart can’t pump enough blood to the lungs to pick up oxygen. Left-side heart failure occurs if the heart can’t pump enough oxygen-rich blood to the rest of the body. Right-side heart failure may cause fluid to build up in the feet, ankles, legs, liver, abdomen, and the veins in the neck. Right-side and left-side heart failure also may cause shortness of breath and fatigue (tiredness). The leading causes of heart failure are diseases that damage the heart. Examples include coronary heart disease (CHD), high blood pressure, and diabetes.
Outlook
Heart failure is a very common condition. About 5.1 million people in the United States have heart failure.
Both children and adults can have the condition, although the symptoms and treatments differ. This article focuses on heart failure in adults. Currently, heart failure has no cure. However, treatments—such as medicines and lifestyle changes—can help people who have the condition live longer and more active lives. Researchers continue to study new ways to treat heart failure and its complications.
Source: National Heart, Lung, and Blood Institute; National Institutes of Health; U.S. Department of Health and Human Services.
Holter and Event Monitors
Event Monitors Event monitors are similar to Holter monitors. You wear one while you do your normal daily activities. Most event monitors have wires that connect the device to sensors. The sensors are stuck to your chest using sticky patches. Unlike Holter monitors, event monitors don’t continuously record your heart’s electrical activity. They only record during symptoms. For many event monitors, you need to start the device when you feel symptoms. Some event monitors start automatically if they detect abnormal heart rhythms.
Event monitors tend to be smaller than Holter monitors because they don’t need to store as much data.
Different types of event monitors work in slightly different ways. Your doctor will explain how to use the monitor before you start wearing it.
Implantable Loop Recorders
You may need an implantable loop recorder if other event monitors can’t provide enough data. Implantable loop recorders are about the size of a pack of gum. This type of event monitor is inserted under the skin on your chest. No wires or chest sensors are used. Your doctor can program the device to record when you start it during symptoms or automatically if it detects an abnormal heart rhythm. Devices may differ, so your doctor will tell you how to use your recorder. Sometimes a special card is held close to the recorder to start it.
Other Names for Holter and Event Monitors
Ambulatory EKG or ECG. (The terms “EKG” and “ECG” both stand for electrocardiogram.)
Continuous EKG or ECG.
EKG event monitors.
Episodic monitors.
Mobile cardiac outpatient telemetry systems. This is another name for autodetect recorders.
Thirty-day event recorders.
Transtelephonic event monitors. These monitors require the patient to send the collected data by telephone to a doctor’s office or a company that checks the data.
Source: National Heart, Lung, and Blood Institute; National Institutes of Health; U.S. Department of Health and Human Services.
Hypertension Clinic
What Is High Blood Pressure?
High blood pressure (HBP) is a serious condition that can lead to coronary heart disease, heart failure, stroke, kidney failure, and other health problems. “Blood pressure” is the force of blood pushing against the walls of the arteries as the heart pumps blood. If this pressure rises and stays high over time, it can damage the body in many ways.
Overview
About 1 in 3 adults in the United States has HBP. The condition itself usually has no signs or symptoms. You can have it for years without knowing it. During this time, though, HBP can damage your heart, blood vessels, kidneys, and other parts of your body. Knowing your blood pressure numbers is important, even when you’re feeling fine. If your blood pressure is normal, you can work with your health care team to keep it that way. If your blood pressure is too high, treatment may help prevent damage to your body’s organs.
Blood Pressure Numbers
Blood pressure is measured as systolic (sis-TOL-ik) and diastolic (di-ah-STOL-ik) pressures. “Systolic” refers to blood pressure when the heart beats while pumping blood. “Diastolic” refers to blood pressure when the heart is at rest between beats. Blood pressure doesn’t stay the same all the time. It lowers as you sleep and rises when you wake up. Blood pressure also rises when you’re excited, nervous, or active. If your numbers stay above normal most of the time, you’re at risk for health problems. The risk grows as blood pressure numbers rise. “Prehypertension” means you may end up with HBP, unless you take steps to prevent it. If you’re being treated for HBP and have repeat readings in the normal range, your blood pressure is under control. However, you still have the condition. You should see your doctor and follow your treatment plan to keep your blood pressure under control.
Outlook
Blood pressure tends to rise with age. Following a healthy lifestyle helps some people delay or prevent this rise in blood pressure. People who have HBP can take steps to control it and reduce their risk for related health problems. Key steps include following a healthy lifestyle, having ongoing medical care, and following your treatment plan. Most adults should have less than one teaspoon, or 2,300 milligrams, of sodium a day. Being active and maintaining a healthy weight also can help you prevent high blood pressure.
Sources: National Center for Health Statistics. (2007–2010). National Health and Nutrition Examination Survey; Centers for Disease Control and Prevention. (2011). Vital signs: prevalence, treatment, and control of hypertension, 1999–2002 and 2005–2008. MMWR: Morbidity & Mortality Weekly Report, 60(4), 103–108; National Heart, Lung, and Blood Institute, National High Blood Pressure Education Program. (2004). The seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure.
Imaging Stress Test
An imaging stress test might be done first (as opposed to a standard exercise stress test) if you:
Can’t exercise for enough time to get your heart working at its hardest. (Medical problems, such as arthritis or leg arteries clogged by plaque, might prevent you from exercising long enough.)
Have abnormal heartbeats or other problems that prevent a standard exercise stress test from giving correct results.
Had a heart procedure in the past, such as coronary artery bypass grafting orangioplasty (AN-jee-oh-plas-tee) and stent placement.
Implantation of Cardiac Pacemakers and Defibrillators
A pacemaker is a small device that’s placed in the chest or abdomen to help control abnormal heart rhythms. This device uses electrical pulses to prompt the heart to beat at a normal rate. Pacemakers are used to treat arrhythmias (ah-RITH-me-ahs). Arrhythmias are problems with the rate or rhythm of the heartbeat. During an arrhythmia, the heart can beat too fast, too slow, or with an irregular rhythm. A heartbeat that’s too fast is called tachycardia (TAK-ih-KAR-de-ah). A heartbeat that’s too slow is called bradycardia (bray-de-KAR-de-ah).
During an arrhythmia, the heart may not be able to pump enough blood to the body. This can cause symptoms such as fatigue (tiredness), shortness of breath, or fainting. Severe arrhythmias can damage the body’s vital organs and may even cause loss of consciousness or death. A pacemaker can relieve some arrhythmia symptoms, such as fatigue and fainting. A pacemaker also can help a person who has abnormal heart rhythms resume a more active lifestyle.
Understanding the Heart’s Electrical System
Your heart has its own internal electrical system that controls the rate and rhythm of your heartbeat. With each heartbeat, an electrical signal spreads from the top of your heart to the bottom. As the signal travels, it causes the heart to contract and pump blood. Each electrical signal normally begins in a group of cells called the sinus node or sinoatrial (SA) node. As the signal spreads from the top of the heart to the bottom, it coordinates the timing of heart cell activity. First, the heart’s two upper chambers, the atria (AY-tree-uh), contract. This contraction pumps blood into the heart’s two lower chambers, the ventricles (VEN-trih-kuls). The ventricles then contract and pump blood to the rest of the body. The combined contraction of the atria and ventricles is a heartbeat.
Overview
Faulty electrical signaling in the heart causes arrhythmias. Pacemakers use low-energy electrical pulses to overcome this faulty electrical signaling.
Pacemakers can:
Speed up a slow heart rhythm.
Help control an abnormal or fast heart rhythm.
Make sure the ventricles contract normally if the atria are quivering instead of beating with a normal rhythm (a condition called atrial fibrillation).
Coordinate electrical signaling between the upper and lower chambers of the heart.
Coordinate electrical signaling between the ventricles. Pacemakers that do this are called cardiac resynchronization therapy (CRT) devices. CRT devices are used to treat heart failure.
Prevent dangerous arrhythmias caused by a disorder called long QT syndrome.
Pacemakers also can monitor and record your heart’s electrical activity and heart rhythm. Newer pacemakers can monitor your blood temperature, breathing rate, and other factors. They also can adjust your heart rate to changes in your activity. Pacemakers can be temporary or permanent. Temporary pacemakers are used to treat short-term heart problems, such as a slow heartbeat that’s caused by a heart attack, heart surgery, or an overdose of medicine. Temporary pacemakers also are used during emergencies. They might be used until your doctor can implant a permanent pacemaker or until a temporary condition goes away. If you have a temporary pacemaker, you’ll stay in a hospital as long as the device is in place. Permanent pacemakers are used to control long-term heart rhythm problems. This article mainly discusses permanent pacemakers, unless stated otherwise.
Doctors also treat arrhythmias with another device called an implantable cardioverter defibrillator (ICD). An ICD is similar to a pacemaker. However, besides using low-energy electrical pulses, an ICD also can use high-energy pulses to treat life-threatening arrhythmias.
What Is an Implantable Cardioverter Defibrillator?
An implantable cardioverter defibrillator (ICD) is a small device that’s placed in the chest or abdomen. Doctors use the device to help treat irregular heartbeats called arrhythmias (ah-RITH-me-ahs). An ICD uses electrical pulses or shocks to help control life-threatening arrhythmias, especially those that can cause sudden cardiac arrest (SCA). SCA is a condition in which the heart suddenly stops beating. If the heart stops beating, blood stops flowing to the brain and other vital organs. SCA usually causes death if it’s not treated within minutes.
Understanding the Heart’s Electrical System
Your heart has its own internal electrical system that controls the rate and rhythm of your heartbeat. With each heartbeat, an electrical signal spreads from the top of your heart to the bottom. As the signal travels, it causes the heart to contract and pump blood. Each electrical signal normally begins in a group of cells called the sinus node or sinoatrial (SA) node. As a signal spreads from the top of the heart to the bottom, it coordinates the timing of heart cell activity. First, the heart’s two upper chambers, the atria (AY-tree-uh), contract. This contraction pumps blood into the heart’s two lower chambers, the ventricles (VEN-trih-kuls). The ventricles then contract and pump blood to the rest of the body. The combined contraction of the atria and ventricles is a heartbeat.
Overview
A problem with any part of the heart’s electrical system can cause an arrhythmia. Most arrhythmias are harmless, but some can be serious. ICDs use electrical pulses or shocks to treat life-threatening arrhythmias that occur in the ventricles (the heart’s lower chambers). When ventricular arrhythmias occur, the heart can’t pump blood well. You can pass out within seconds and die within minutes if not treated. To prevent death, the arrhythmia must be treated right away with an electric shock to the heart. This treatment is called defibrillation (de-fib-ri-LA-shun). An ICD has wires with electrodes on the ends that connect to your heart chambers. The ICD will monitor your heart rhythm. If the device detects an irregular rhythm in your ventricles, it will use low-energy electrical pulses to restore a normal rhythm. If the low-energy pulses don’t restore your normal heart rhythm, the ICD will switch to high-energy pulses for defibrillation. The device also will switch to high-energy pulses if your ventricles start to quiver rather than contract strongly. The high-energy pulses last only a fraction of a second, but they can be painful. Doctors also treat arrhythmias with another device called a pacemaker. An ICD is similar to a pacemaker, but has some differences. Pacemakers give off only low-energy electrical pulses. They’re often used to treat less dangerous heart rhythms, such as those that occur in the upper chambers of your heart. Most new ICDs can act as both pacemakers and defibrillators.
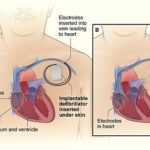 Comparison of an Implantable Cardioverter Defibrillator and a Pacemaker The image compares an ICD with a pacemaker. Figure A shows the location and general size of an ICD in the upper chest. The wires with electrodes on the ends are inserted into the heart through a vein in the upper chest. Figure B shows the location and general size of a pacemaker in the upper chest. The wires with electrodes on the ends are inserted into the heart through a vein in the upper chest. People who have heart failure may need a special device called a cardiac resynchronization therapy (CRT) device. The CRT device is able to pace both ventricles at the same time. This allows them to work together and do a better job pumping blood out of the heart. CRT devices that have a defibrillator are called CRT-D.
Comparison of an Implantable Cardioverter Defibrillator and a Pacemaker The image compares an ICD with a pacemaker. Figure A shows the location and general size of an ICD in the upper chest. The wires with electrodes on the ends are inserted into the heart through a vein in the upper chest. Figure B shows the location and general size of a pacemaker in the upper chest. The wires with electrodes on the ends are inserted into the heart through a vein in the upper chest. People who have heart failure may need a special device called a cardiac resynchronization therapy (CRT) device. The CRT device is able to pace both ventricles at the same time. This allows them to work together and do a better job pumping blood out of the heart. CRT devices that have a defibrillator are called CRT-D.
Source: National Heart, Lung, and Blood Institute; National Institutes of Health; U.S. Department of Health and Human Services.
Nuclear Stress Test – (Single Photo Emission Computed Tomography)
Doctors use SPECT to help diagnose coronary heart disease (CHD). Combining SPECT with a stress test can show problems with blood flow to the heart. Sometimes doctors can detect these problems only when the heart is working hard and beating fast. Doctors also use SPECT to look for areas of damaged or dead heart muscle tissue. These areas might be the result of a previous heart attack or other cause. SPECT also can show how well the heart’s lower left chamber (left ventricle) pumps blood to the body. Weak pumping ability might be the result of a heart attack, heart failure, and other causes.
Tracers commonly used during SPECT include thallium-201, technetium-99m sestamibi (Cardiolite®), and technetium-99m tetrofosmin (Myoview™).
Source: National Heart, Lung, and Blood Institute; National Institutes of Health; U.S. Department of Health and Human Services.
Peripheral Vascular Disease Testing
Specialists Involved
Primary care doctors, such as internists and family doctors, may treat people who have mild P.A.D. For more advanced P.A.D., a vascular specialist may be involved. This is a doctor who specializes in treating blood vessel diseases and conditions. A cardiologist also may be involved in treating people who have P.A.D. Cardiologists treat heart problems, such as CHD and heart attack, which often affect people who have P.A.D.
Medical and Family Histories
Your doctor may ask:
Whether you have any risk factors for P.A.D. For example, he or she may ask whether you smoke or have diabetes.
About your symptoms, including any symptoms that occur when walking, exercising, sitting, standing, or climbing.
About your diet.
About any medicines you take, including prescription and over-the-counter medicines.
Whether anyone in your family has a history of heart or blood vessel diseases.
Physical Exam
During the physical exam, your doctor will look for signs of P.A.D. He or she may check the blood flow in your legs or feet to see whether you have weak or absent pulses. Your doctor also may check the pulses in your leg arteries for an abnormal whooshing sound called a bruit (broo-E). He or she can hear this sound with a stethoscope. A bruit may be a warning sign of a narrowed or blocked artery. Your doctor may compare blood pressure between your limbs to see whether the pressure is lower in the affected limb. He or she also may check for poor wound healing or any changes in your hair, skin, or nails that may be signs of P.A.D.
Diagnostic Tests
Ankle-Brachial Index
A simple test called an ankle-brachial index (ABI) often is used to diagnose P.A.D. The ABI compares blood pressure in your ankle to blood pressure in your arm. This test shows how well blood is flowing in your limbs.
ABI can show whether P.A.D. is affecting your limbs, but it won’t show which blood vessels are narrowed or blocked. A normal ABI result is 1.0 or greater (with a range of 0.90 to 1.30). The test takes about 10 to 15 minutes to measure both arms and both ankles. This test may be done yearly to see whether P.A.D. is getting worse.
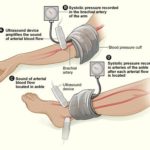 The illustration shows the ankle-brachial index test. The test compares blood pressure in the ankle to blood pressure in the arm. As the blood pressure cuff deflates, the blood pressure in the arteries is recorded.
The illustration shows the ankle-brachial index test. The test compares blood pressure in the ankle to blood pressure in the arm. As the blood pressure cuff deflates, the blood pressure in the arteries is recorded.
Doppler Ultrasound
A Doppler ultrasound looks at blood flow in the major arteries and veins in the limbs. During this test, a handheld device is placed on your body and passed back and forth over the affected area. A computer converts sound waves into a picture of blood flow in the arteries and veins. The results of this test can show whether a blood vessel is blocked. The results also can help show the severity of P.A.D.
Phlebectomy
You’ll be awake during the procedure, but your doctor will numb the area around the vein. Usually, you can go home the same day that the procedure is done.
Source: National Heart, Lung, and Blood Institute; National Institutes of Health; U.S. Department of Health and Human Services.
Radio Frequency Ablation
Radial Cardiac Catheterization
Right Heart Catheterization
In a right-heart catheterization, your doctor guides a special catheter (a small, hollow tube) called a pulmonary artery (PA) catheter to the right side of your heart. He or she then passes the tube into your pulmonary artery. This is the main artery that carries blood to your lungs. Your doctor observes blood flow through your heart and measures the pressures inside your heart and lungs. As the catheter advances toward your pulmonary artery, your doctor measures pressures along the way, inside the chambers on the right side of your heart. This includes the right atrium and right ventricle. Your doctor can also take indirect measurements of pressures on the left side of your heart. Your cardiac output—the amount of blood your heart pumps per minute—is also determined during a right-heart catheterization. All of these measurements are used to diagnose heart conditions and to determine what treatment might be right for you.
You might need a right-heart catheterization to diagnose or manage Heart failure, Heart valve disease, cardiomyopathy, and Pulmonary hypertension.
Sclerotherapy
This procedure often is used to treat smaller varicose veins and spider veins. It can be done in your doctor’s office, while you stand. You may need several treatments to completely close off a vein.
Treatments typically are done every 4 to 6 weeks. Following treatments, your legs will be wrapped in elastic bandaging to help with healing and decrease swelling.
Source: National Heart, Lung, and Blood Institute; National Institutes of Health; U.S. Department of Health and Human Services.
Transthoracic and Transesophageal Echocardiography
There are several types of echocardiography (echo)—all use sound waves to create moving pictures of your heart. This is the same technology that allows doctors to see an unborn baby inside a pregnant woman. Unlike x rays and some other tests, echo doesn’t involve radiation.
Transthoracic Echocardiography
Transthoracic (tranz-thor-AS-ik) echo is the most common type of echocardiogram test. It’s painless and noninvasive. “Noninvasive” means that no surgery is done and no instruments are inserted into your body. This type of echo involves placing a device called a transducer on your chest. The device sends special sound waves, called ultrasound, through your chest wall to your heart. The human ear can’t hear ultrasound waves. As the ultrasound waves bounce off the structures of your heart, a computer in the echo machine converts them into pictures on a screen.
Transesophageal Echocardiography
Your doctor may have a hard time seeing the aorta and other parts of your heart using a standard transthoracic echo. Thus, he or she may recommend transesophageal (tranz-ih-sof-uh-JEE-ul) echo, or TEE. During this test, the transducer is attached to the end of a flexible tube. The tube is guided down your throat and into your esophagus (the passage leading from your mouth to your stomach). This allows your doctor to get more detailed pictures of your heart.
What Is Transesophageal Echocardiography?
Transesophageal (tranz-ih-sof-uh-JEE-ul) echocardiography (EK-o-kar-de-OG-rah-fee), or TEE, is a test that uses sound waves to create high-quality moving pictures of the heart and its blood vessels. TEE is a type of echocardiography (echo). Echo shows the size and shape of the heart and how well the heart chambers and valves are working. Echo can pinpoint areas of heart muscle that aren’t contracting well because of poor blood flow or injury from a previous heart attack. Echo also can detect possible blood clots inside the heart, fluid buildup in the pericardium (the sac around the heart), and problems with the aorta. The aorta is the main artery that carries oxygen-rich blood from your heart to your body.
Overview
During echo, a device called a transducer is used to send sound waves (called ultrasound) to the heart. As the ultrasound waves bounce off the structures of the heart, a computer in the echo machine converts them into pictures on a screen. TEE involves a flexible tube (probe) with a transducer at its tip. Your doctor will guide the probe down your throat and into your esophagus (the passage leading from your mouth to your stomach). This approach allows your doctor to get more detailed pictures of your heart because the esophagus is directly behind the heart. TEE can help doctors diagnose heart and blood vessel diseases and conditions in adults and children. Doctors also may use TEE to guide cardiac catheterization (KATH-eh-ter-ih-ZA-shun), help prepare for surgery, or assess a patient’s status during or after surgery. Doctors may use TEE in addition to transthoracic (tranz-thor-AS-ik) echo (TTE), the most common type of echo. If TTE pictures don’t give doctors enough information, they may recommend TEE to get more detailed pictures.
Outlook
TEE has a low risk of complications in both adults and children. Even newborns can have TEE.
Source: National Heart, Lung, and Blood Institute; National Institutes of Health; U.S. Department of Health and Human Services.
Venous treatment/ablation
Your doctor makes a tiny cut in your skin near the varicose vein. He or she then inserts a small tube called a catheter into the vein. A device at the tip of the tube heats up the inside of the vein and closes it off.
You’ll be awake during this procedure, but your doctor will numb the area around the vein. You usually can go home the same day as the procedure.
Source: National Heart, Lung, and Blood Institute; National Institutes of Health; U.S. Department of Health and Human Services.
Statesboro’s Trusted Cardiac, Vascular & Vein Specialists
Located at our 5 Grady Johnson Road office location and staffed daily by one of our cardiologists, we offer our patients appointments for urgent cardiac or peripheral vascular concerns, pre-operative clearance and noninvasive testing.

